-
 Overview
Overview
A hammertoe is a toe that's curled due to a bend in the middle joint of a toe. Mallet toe is similar, but affects the upper joint of a toe. Otherwise, any differences between Hammertoes and mallet toe are subtle. Both hammertoe and mallet toe are commonly caused by shoes that are too short or heels that are too high. Under these conditions, your toe may be forced against the front of your shoe, resulting in an unnatural bending of your toe and a hammer-like or claw-like appearance. Relieving the pain and pressure of hammertoe and mallet toe may involve changing your footwear and wearing shoe inserts. If you have a more severe case of hammertoe or mallet toe, you may need surgery to experience relief.
Causes
Many disorders can affect the joints in the toes, causing pain and preventing the foot from functioning as it should. A mallet toe occurs when the joint at the end of the toe cannot straighten. Excessive rubbing of the mallet toe against the top of the shoe can lead to pain and the development of a corn. The tip of the toe is often turned down against the shoe causing pressure and discomfort. Arthritis can also lead to many forefoot deformities including mallet toes. Mallet toes can cause extreme discomfort, and can be aggravated if restrictive or improperly fitting footwear is worn for a prolonged period of time.
Symptoms
Well-developed hammertoes are distinctive due to the abnormal bent shape of the toe. However, there are many other common symptoms. Some symptoms may be present before the toe becomes overly bent or fixed in the contracted position. Often, before the toe becomes permanently contracted, there will be pain or irritation over the top of the toe, particularly over the joint. The symptoms are pronounced while wearing shoes due to the top of the toe rubbing against the upper portion of the shoe. Often, there is a significant amount of friction between the toe and the shoe or between the toe and the toes on either side of it. The corns may be soft or hard, depending on their location and age. The affected toe may also appear red with irritated skin. In more severe cases, blisters or open sores may form. Those with diabetes should take extra care if they develop any of these symptoms, as they could lead to further complications.
Diagnosis
The exam may reveal a toe in which the near bone of the toe (proximal phalanx) is angled upward and the middle bone of the toe points in the opposite direction (plantar flexed). Toes may appear crooked or rotated. The involved joint may be painful when moved, or stiff. There may be areas of thickened skin (corns or calluses) on top of or between the toes, a callus may also be observed at the tip of the affected toe beneath the toenail. An attempt to passively correct the deformity will help elucidate the best treatment option as the examiner determines whether the toe is still flexible or not. It is advisable to assess palpable pulses, since their presence is associated with a good prognosis for healing after surgery. X-rays will demonstrate the contractures of the involved joints, as well as possible arthritic changes and bone enlargements (exostoses, spurs). X-rays of the involved foot are usually performed in a weight-bearing position.
Non Surgical Treatment
Your podiatrist may recommend one or more of these treatments to manage your hammer toes. Wear shoes with roomy toe boxes which don?t force your toes together. Exercises to stretch and strengthen muscles in the toes. Over the counter toe straps, cushions, and corn pads. Custom orthotic inserts. Toe caps or toe slings. In severe cases, surgery to release the muscles in the affected toes.
Surgical Treatment
For the surgical correction of a rigid hammertoe, the surgical procedure consists of removing the damaged skin where the corn is located. Then a small section of bone is removed at the level of the rigid joint. The sutures remain in place for approximately ten days. During this period of time it is important to keep the area dry. Most surgeons prefer to leave the bandage in place until the patient's follow-up visit, so there is no need for the patient to change the bandages at home. The patient is returned to a stiff-soled walking shoe in about two weeks. It is important to try and stay off the foot as much as possible during this time. Excessive swelling of the toe is the most common patient complaint. In severe cases of hammertoe deformity a pin may be required to hold the toe in place and the surgeon may elect to fuse the bones in the toe. This requires several weeks of recovery.
-
Overview
Heel Pain may develop when you pound your feet on hard surfaces playing sports or wear shoes that irritate sensitive tissues. A sore heel will usually get better on its own if you give it enough rest. Unfortunately, many people try to ignore the early signs of heel pain and keep on doing the activities that caused it and this can lead to chronic pain. Conditions that cause heel pain generally fall into two main categories: pain beneath the heel and pain behind the heel. Pain beneath the Heel. If it hurts under your heel, you may have one or more conditions that cause inflammation of the tissues on the bottom of your foot. Stone bruise. By stepping on a hard object, you can bruise the fat pad on the bottom side of your heel. It may or may not look discoloured. With rest, the pain subsides gradually.
Causes
As stated above, if biomechanical complaints such as over pronation exist during running then this can lead to planter fascitis and heel pain. Over pronation occurs when there is excessive mobility in the sab-taler joint of the foot which causes hyper mobility of the foot. Conditions such as flat feet can also cause over pronation. This increased mobility adversely affects all the muscles in the foot and can even affect the lower leg, upper leg and cause back pain. The mechanical imbalance is highlighted during running due to the increased forces being applied to the body Runners often complain that the pain increases when they enter the toe off phase of the running cycle as this stretches the muscle away from the heel bone. Apart from over pronation, other causes of planter fascitis are a change of running shoes, dramatic increases in speed work, hill work and mileage.
Symptoms
Depending on the specific form of heel pain, symptoms may vary. Pain stemming from plantar fasciitis or heel spurs is particularly acute following periods of rest, whether it is after getting out of bed in the morning, or getting up after a long period of sitting. In many cases, pain subsides during activity as injured tissue adjusts to damage, but can return again with prolonged activity or when excessive pressure is applied to the affected area. Extended periods of activity and/or strain of the foot can increase pain and inflammation in the foot. In addition to pain, heel conditions can also generate swelling, bruising, and redness. The foot may also be hot to the touch, experience tingling, or numbness depending on the condition.
Diagnosis
The diagnosis of heel pain and heel spurs is made by a through history of the course of the condition and by physical exam. Weight bearing x-rays are useful in determining if a heel spur is present and to rule out rare causes of heel pain such as a stress fracture of the heel bone, the presence of bone tumors or evidence of soft tissue damage caused by certain connective tissue disorders.
Non Surgical Treatment
Physical medicine modalities are well known for their benefits and they have been consistently applied in early treatment of plantar fasciitis. Typically, the direct application of ice, ice baths or contrast soaking aid in the local reduction of inflammation and temporarily augment pain management. Electric stimulation may only provide indirect reduction of interstitial inflammation of the plantar fascia. Ultrasound therapy, hot pack systems and deep tissue massage help eliminate inflammation and aid in restoring plantar fascia tensegrity. Generally, these modalities are considered to be valuable adjuncts to a well-organised treatment plan. Various programs of stretching, range of motion and therapeutic exercises can help re-establish foot function and improve tolerance to load. When it is done appropriately, stretching can serve as an important adjunct to the resumption of the plantar fascia?s ability to tolerate eccentric loading forces that typically occur during stance and gait. Night splinting has proven to be an effective tool in managing persistent plantar fasciitis. Antiinflammatory modalities, such as ice and ice baths, are often the first line of treatment. Oral NSAIDs have been a mainstay of treatment. While they effectively relieve symptoms, be aware that they frequently fail to promote sustained relief. When inflammation is severe or fails to respond to initial efforts, one may consider corticosteroid injection(s). However, keep in mind that corticosteroid injections impose the risk of aponeurosis rupture secondary to focal collagen tissue necrosis and can result in focal heel fat pad atrophy.
Surgical Treatment
At most 95% of heel pain can be treated without surgery. A very low percentage of people really need to have surgery on the heel. It is a biomechanical problem and it?s very imperative that you not only get evaluated, but receive care immediately. Having heel pain is like having a problem with your eyes; as you would get glasses to correct your eyes, you should look into orthotics to correct your foot. Orthotics are sort of like glasses for the feet. They correct and realign the foot to put them into neutral or normal position to really prevent heel pain, and many other foot issues. Whether it be bunions, hammertoes, neuromas, or even ankle instability, a custom orthotic is something worth considering.
Prevention
A variety of steps can be taken to avoid heel pain and accompanying afflictions. Wear shoes that fit well-front, back, and sides-and have shock-absorbent soles, rigid shanks, and supportive heel counters. Wear the proper shoes for each activity. Do not wear shoes with excessive wear on heels or soles. Prepare properly before exercising. Warm up and do stretching exercises before and after running. Pace yourself when you participate in athletic activities. Don't underestimate your body's need for rest and good nutrition. If obese, lose weight. 2643 commentaires
2643 commentaires
-
These doctors can offer an array of options to help ease your pain. You may get a cortisone shot, but this is only a temporary solution. Also, some doctors will tell you to use pain medication, such as ibuprofen or some other anti-inflammatory medicine. Furthermore , physical therapy can also help since this will help diminish stiffness. The most common form of investigation is a radiological imaging study. These include weight bearing, oblique, and lateral as well as anteroposterior radiographs. The radiographs are taken and the measurement of Hallux abductus angle, intermetatarsal angle, medial prominence of the first metatarsal head and congruency of the metatarsophalageal (MTP joint) are taken. In conclusion, the fundamental poses of hatha yoga provide an opportunity for a complete workout for your feet that is highly effective for preventing, slowing, and even halting the progress of bunions. It takes a little extra effort and attention, but your practice as a whole will benefit from it, even if your feet don’t (yet) show any signs of bunions. When you add a little warm-up and workout for your arches and toes, yoga will keep your feet happy and healthy. As you’re stretching see if you can see the “knuckles of the foot” like you would see the knuckles of your hand if you made a fist. Foot Pain from bunions is a very common complaint at my office. I once had a distasteful dream about a bunion. In this "work-mare" my foot had a bunion that kept getting bigger and bigger each time I looked at it. Perhaps I see too many bunions from day to day. However, I am surprised that many of my patients do not even know what bunions are or what causes them. Simply stated, a bunion is a bump at the base and side of the great toe There are some exercises and alternative bunion pain relief provided by alternative medicine that you can choose upon as follows. There are some habits that can be started or changed to help eliminate bunion discomfort. Along with avoiding pointed or narrow toes, one can also go for padding especially in the location of the bunion to reduce the bunion discomfort. Such pads are stocked at convenience stores or at normal shoe producers too. The level of activity of the feet, their age, and the degree of the malformation are all considered by the ankle surgeon before deciding upon the correct method to go about it. Bunions pain can be eliminated permanently via surgery, but the discomfort itself can be made less by using medications, massage and less movement. In arthritic conditions, especially rheumatoid arthritis, it is important to establish a correct diagnosis. Often the symptoms in the foot or ankle may be the first indications of this diagnosis. A diagnosis is obtained through review of your medical history, your current occupation, and recreations activities you participate in and any previous history of problems to your feet or legs. One possible indication of RA is appearance of symptoms in the same joint on both feet or several joints in the feet. X-rays may also be obtained to clarify what joint damage is occurring.
 Finding a good surgeon isn't too difficult. You'll be looking for a podiatrist, and you can usually find one through a quick session of online research. Basically you should look at education, experience, and proximity to you. You can also take a look at comments from previous patients since they often get online and post reviews and comments about their experiences. In other words, it's a kind of digital word of mouth that can go a long way towards helping you find the best surgeon possible. They'll explain your options and let you know if the surgery is right for you. Bunions are bumps at the base of the big toe, on the outer side of the toe. They form when the big toe turns inward toward the second toe, gradually altering the big toe's skeletal structure, explains the American College of Foot and Ankle Surgeons. The angle of the bone causes a protrusion, and inflammation and pain may result. Bunions can make running particularly painful and difficult. Causes Ill-fitting shoes, particularly those with tight toe boxes, create friction and pressure on toes, aggravating bunions and causing pain while running. Running also increases repetitive pressure on the big toe's joint and the ball of the foot, another source of bunion pain. Surgery is recommended when one is experiencing severe and persistent pain. Sometimes the tendons and ligaments around the affected big toe may need to be repaired. To prevent the big toe from angling towards the second toe, some tissues might have to be loosened and some might have to be lengthened. Arthrodesis is one procedure where the damaged joint surfaces need to be removed and then screws, plates and wires are inserted to hold the joint together till it heals completely. If there is no angulation, the bump on the joint might be simply removed. This procedure is referred to as exostectomy. A bunion looks like a "bump" on the joint of the big toe; however, these bumps are not calluses. Instead they result from the bones in your foot becoming misaligned. More often than not, the big toe is leaning inward towards the middle toe giving the appearance of a bump on the joint. Bunions are a progressive disease that warrants treatment by a Boston podiatry specialist or foot doctor early on. read more Ever flinched because your bunions have made walking painful? You're not alone. Depending on how severe the deformity is, a bunion can make simple activities like walking and running both painful and tiring. read more The purpose of this article is to provide an outline of common foot disorders. The ultimate message is to take care of foot problems as they arise in a timely manner so they do not get worse. Your feet are your wheels, and if they are not working as they should, you’re grounded. Be sure to discuss any foot problems you may be having with your doctor. This is especially true if your foot problems are related to chronic medical conditions like rheumatoid arthritis, diabetes, or peripheral artery disease. Cold press may be applied to the affected area to reduce swelling. Proper rest and proper stride can help as well.
Finding a good surgeon isn't too difficult. You'll be looking for a podiatrist, and you can usually find one through a quick session of online research. Basically you should look at education, experience, and proximity to you. You can also take a look at comments from previous patients since they often get online and post reviews and comments about their experiences. In other words, it's a kind of digital word of mouth that can go a long way towards helping you find the best surgeon possible. They'll explain your options and let you know if the surgery is right for you. Bunions are bumps at the base of the big toe, on the outer side of the toe. They form when the big toe turns inward toward the second toe, gradually altering the big toe's skeletal structure, explains the American College of Foot and Ankle Surgeons. The angle of the bone causes a protrusion, and inflammation and pain may result. Bunions can make running particularly painful and difficult. Causes Ill-fitting shoes, particularly those with tight toe boxes, create friction and pressure on toes, aggravating bunions and causing pain while running. Running also increases repetitive pressure on the big toe's joint and the ball of the foot, another source of bunion pain. Surgery is recommended when one is experiencing severe and persistent pain. Sometimes the tendons and ligaments around the affected big toe may need to be repaired. To prevent the big toe from angling towards the second toe, some tissues might have to be loosened and some might have to be lengthened. Arthrodesis is one procedure where the damaged joint surfaces need to be removed and then screws, plates and wires are inserted to hold the joint together till it heals completely. If there is no angulation, the bump on the joint might be simply removed. This procedure is referred to as exostectomy. A bunion looks like a "bump" on the joint of the big toe; however, these bumps are not calluses. Instead they result from the bones in your foot becoming misaligned. More often than not, the big toe is leaning inward towards the middle toe giving the appearance of a bump on the joint. Bunions are a progressive disease that warrants treatment by a Boston podiatry specialist or foot doctor early on. read more Ever flinched because your bunions have made walking painful? You're not alone. Depending on how severe the deformity is, a bunion can make simple activities like walking and running both painful and tiring. read more The purpose of this article is to provide an outline of common foot disorders. The ultimate message is to take care of foot problems as they arise in a timely manner so they do not get worse. Your feet are your wheels, and if they are not working as they should, you’re grounded. Be sure to discuss any foot problems you may be having with your doctor. This is especially true if your foot problems are related to chronic medical conditions like rheumatoid arthritis, diabetes, or peripheral artery disease. Cold press may be applied to the affected area to reduce swelling. Proper rest and proper stride can help as well.
-
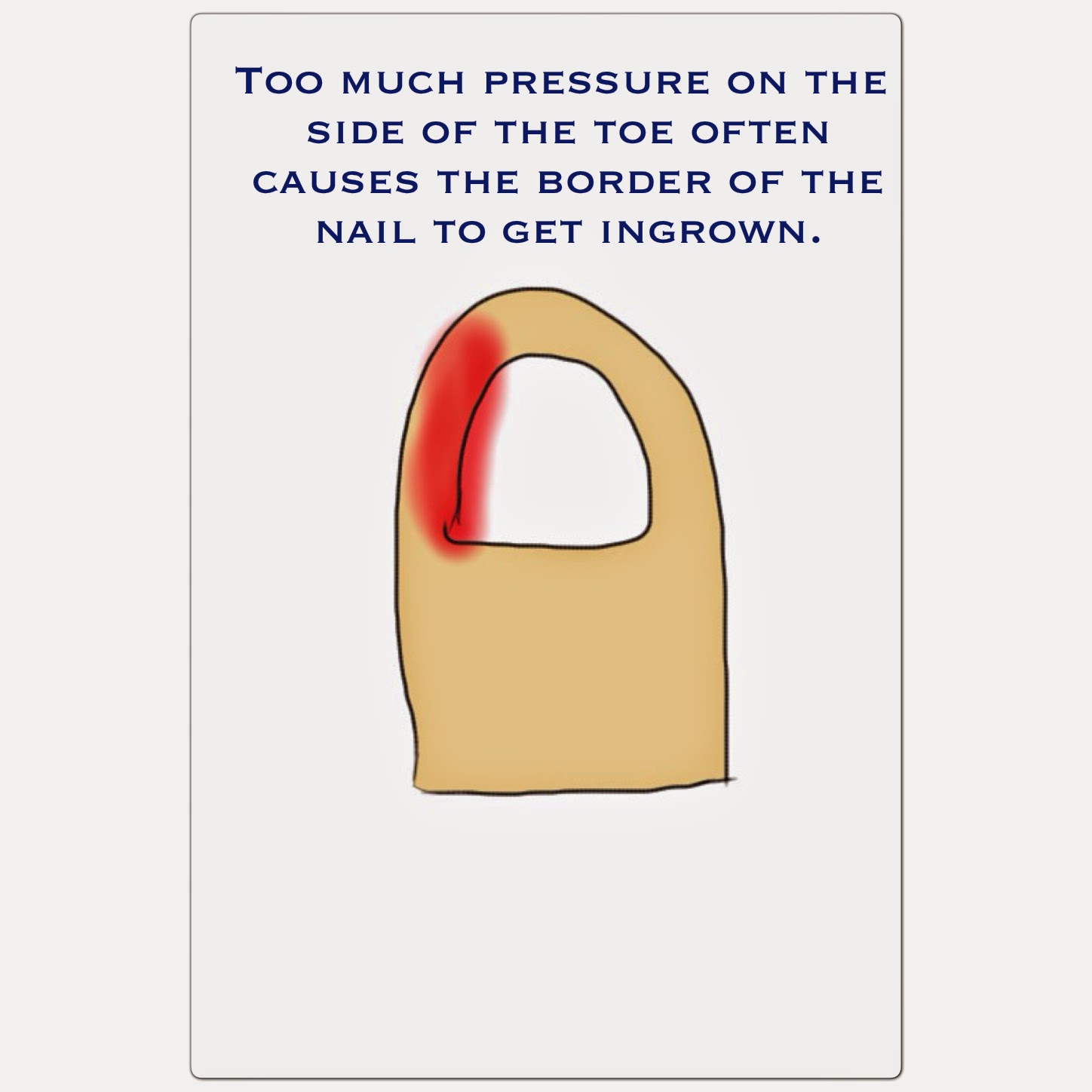
Always wear some type of protection between your feet and your shoes whether you prefer socks, hose, or booties. They have both foot nylons and thin cotton socks that shouldn't show when you have your shoes on depending on the styles. Change your socks at least daily and always keep your feet and socks dry. Avoid foot fungi by wearing skid-proof foot protection in public showers or wet areas, be sure to remember to dry under and between toes, and use appropriate anti-fungal cream or spray at the first sign of rash or itching. Because of this, you have to check your feet at least once every single day. Otherwise, a minor blister, open sore or ingrown toenail can start with a small infection and quickly get much worse. As the bacteria divide, the sharks can do nothing to stop them. In a normal healthy adult, an ingrown toenail can remain infected for days before the infection worsens. In a diabetic, this is simply not true. the Immune system is impaired and ineffective in a diabetic. The disabled immune system is incapable of controlling the growth of the bacteria and serious complications develop. Always wear appropriate diabetic shoes or slippers as well as NEVER walk around barefoot. Deciding on the right shoes is important to foot health and wellness as the majority of diabetic foot injuries are the result of poor fitting footwears. Footwears for diabetics must not be as well tight or narrow. They should be built from comfortable, breathable material and attribute mesh vents to ventilate the shoes, reducing wetness, which tends to reproduced bacteria. Pair a high quality set of diabetic shoes with smooth socks or compression stockings. Cut nails carefully—and straight across. Also, file the edges. Don't cut them too short, since this could lead to ingrown toe nails.
 Wash your feet in lukewarm (not hot!) water. Keep your feet clean by washing them daily. But only use lukewarm water—the temperature you'd use on a newborn baby. Be gentle when bathing your feet. Wash them using a soft washcloth or sponge. Dry by blotting or patting—and make sure to carefully dry between the toes. Moisturize your feet—but not between your toes. Use a moisturizer daily to keep dry skin from itching or cracking. But DON'T moisturize between the toes—this could encourage a fungal infection. Be gentle when bathing your feet. Wash them using a soft washcloth or sponge. Dry by blotting or patting, and carefully dry between the toes. Keep blood sugar level in target range - Your primary care physician can assist you with this, but it's vital that you monitor your blood sugar level closely between visits. Remember, it is problems with your blood sugar level that can cause the damage to blood vessels and nerves that can be so detrimental to your overall health (and your feet in particular). Keeping that level in check can prevent a whole host of other problems. Leg rash and low blood sugar, is where the former is a symptom as a result of hypoglycemia. The following are the two most highly witnessed problems when it comes to one's feet area. By the very process of ‘reflexing’ the feet, Reflexology has been beneficial in aiding the circulation thereby facilitating the healing of ulcers, lack of feeling and cold feet. In many cases the burning pain and numbness due to Peripheral Neuropathy is decreased or at least made somewhat livable with Reflexology sessions done on a regular basis. Candida albicans is a fungus that is responsible for most of the skin infections in people with diabetes. Mucormycosis is a fatal fungal infection that starts at the nose and spreads to the ears and brains. Fungal infections can be cured with the proper medication to kill the fungus.
Wash your feet in lukewarm (not hot!) water. Keep your feet clean by washing them daily. But only use lukewarm water—the temperature you'd use on a newborn baby. Be gentle when bathing your feet. Wash them using a soft washcloth or sponge. Dry by blotting or patting—and make sure to carefully dry between the toes. Moisturize your feet—but not between your toes. Use a moisturizer daily to keep dry skin from itching or cracking. But DON'T moisturize between the toes—this could encourage a fungal infection. Be gentle when bathing your feet. Wash them using a soft washcloth or sponge. Dry by blotting or patting, and carefully dry between the toes. Keep blood sugar level in target range - Your primary care physician can assist you with this, but it's vital that you monitor your blood sugar level closely between visits. Remember, it is problems with your blood sugar level that can cause the damage to blood vessels and nerves that can be so detrimental to your overall health (and your feet in particular). Keeping that level in check can prevent a whole host of other problems. Leg rash and low blood sugar, is where the former is a symptom as a result of hypoglycemia. The following are the two most highly witnessed problems when it comes to one's feet area. By the very process of ‘reflexing’ the feet, Reflexology has been beneficial in aiding the circulation thereby facilitating the healing of ulcers, lack of feeling and cold feet. In many cases the burning pain and numbness due to Peripheral Neuropathy is decreased or at least made somewhat livable with Reflexology sessions done on a regular basis. Candida albicans is a fungus that is responsible for most of the skin infections in people with diabetes. Mucormycosis is a fatal fungal infection that starts at the nose and spreads to the ears and brains. Fungal infections can be cured with the proper medication to kill the fungus.
-
It's not hard to determine the presence of corns, as they appear on those areas of the foot that comes in direct contact with the footwear and is under constant pressure, and these areas typically include sole, toe, the ball of the foot or the outside toe with thick, hard skin There are soft corns and hard ones. Soft corns occur between the toes and appear as simply white hard skin ; otherwise, a normal corn is roundish, white and quite hard to the touch. In older adults, calluses develop because the skin becomes weak and begins to sag. This causes the collection of skin and results in calluses. Treatment A bunion looks like a "bump" on the joint of the big toe; however, these bumps are not calluses. Instead they result from the bones in your foot becoming misaligned. More often than not, the big toe is leaning inward towards the middle toe giving the appearance of a bump on the joint. Bunions are a progressive disease that warrants treatment by a Boston podiatry specialist or foot doctor early on. read more You can spot a bunion a mile away it is a big lump on the side of your foot on the big toe. It is a structured deformity of the bones and joint on the big toe.
 Taking a closer look at our feet can be depressing. Statistically, eight out of every ten adults have calluses, bunions, and corns to deal with. Blisters are a common occurrence as the latest shoe fashions are broken in. Athletically inclined adults (or adults with athletically inclined family members) run a high risk of struggling with athlete’s foot. Depending on how careful you are with pedicures, you can also be subject to painful ingrown nails that can become infected and swollen! For more information about feet or to find a podiatrist in your area, contact the American Podiatric Medical Association at (800) FOOTCARE (366-8227) or visit their Web site at www.apma.org. There are ways to prevent these problems from occurring and there are solutions to most of these foot infirmities, but some are going to be hard to adopt and adapt to your lifestyle. Try to stick with it though, because soft, smooth feet, without squished toes and lumps and bumps, are definitely the way to go! Calluses are larger, and almost always are a painless thickening of skin caused by repeated pressure or irritation on the heels or balls of the feet. Calluses can become painful when they become so dry and cracked that the area becomes sore and tender to the touch. Alison lurched out of her cube and grabbed the sides of her huge foot with both hands. She looked shocked and in pain as she tugged at her foot until the weight came off of it. The whole front of her foot down into her nails was pink from pain. She sat down heavily on the floor, all her attention on her stomped foot. Alison looked extremely hurt by what he had said. She looked sadly down at the huge and still swelling foot in her hands, as if resentful of the huge feet nature had given her.
Taking a closer look at our feet can be depressing. Statistically, eight out of every ten adults have calluses, bunions, and corns to deal with. Blisters are a common occurrence as the latest shoe fashions are broken in. Athletically inclined adults (or adults with athletically inclined family members) run a high risk of struggling with athlete’s foot. Depending on how careful you are with pedicures, you can also be subject to painful ingrown nails that can become infected and swollen! For more information about feet or to find a podiatrist in your area, contact the American Podiatric Medical Association at (800) FOOTCARE (366-8227) or visit their Web site at www.apma.org. There are ways to prevent these problems from occurring and there are solutions to most of these foot infirmities, but some are going to be hard to adopt and adapt to your lifestyle. Try to stick with it though, because soft, smooth feet, without squished toes and lumps and bumps, are definitely the way to go! Calluses are larger, and almost always are a painless thickening of skin caused by repeated pressure or irritation on the heels or balls of the feet. Calluses can become painful when they become so dry and cracked that the area becomes sore and tender to the touch. Alison lurched out of her cube and grabbed the sides of her huge foot with both hands. She looked shocked and in pain as she tugged at her foot until the weight came off of it. The whole front of her foot down into her nails was pink from pain. She sat down heavily on the floor, all her attention on her stomped foot. Alison looked extremely hurt by what he had said. She looked sadly down at the huge and still swelling foot in her hands, as if resentful of the huge feet nature had given her. Suivre le flux RSS des articles
Suivre le flux RSS des articles Suivre le flux RSS des commentaires
Suivre le flux RSS des commentaires


